New therapeutic approach for chronic wounds
02/03/2026A certain bacterium can slow down the healing of chronic wounds. A team from the University Hospital of Würzburg has now found a promising approach to combat the bacterium.
Chronic wounds are becoming an increasingly important health challenge in Germany. It is estimated that one to two million people already suffer from wounds with delayed or no healing. The majority of those affected are older people and people with at least two chronic illnesses. Due to demographic change and an ageing population, the incidence is expected to continue to rise.
Factors such as diabetes, circulatory disorders or pressure loads often prevent a normal healing cascade, so that the wound remains stuck in a permanent inflammatory or repair stage. Bacteria can also delay wound healing.
Biofilm formation as an obstacle to wound healing
The bacterium Pseudomonas aeruginosa is particularly problematic, as it has the ability to form biofilms and therefore significantly delays the healing of chronic wounds. The biofilm acts like a protective barrier and prevents the germs from being reached and destroyed by immune cells, antibiotics or antiseptics.
In addition, the germ continuously releases pro-inflammatory substances and toxins in the biofilm, which keeps the wound in a persistent inflammatory phase. The rod-shaped bacterium produces enzymes and proteases that break down tissue and damage important cells for wound healing.
After one to two weeks, new, healthy tissue appeared
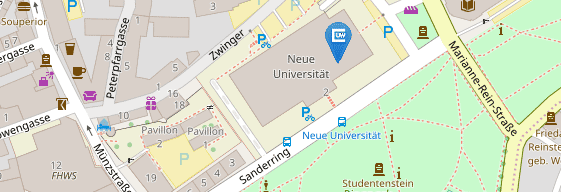
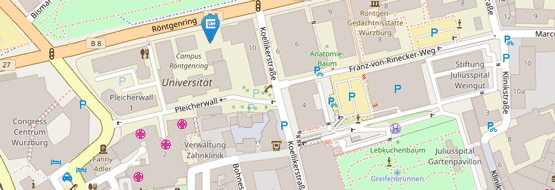
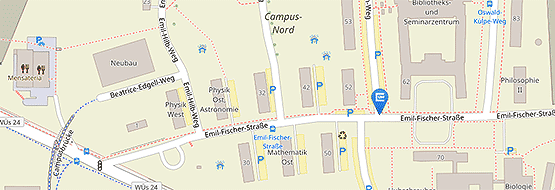
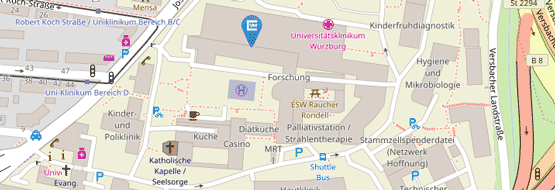
A team from the Clinic and Polyclinic for Dermatology, Venereology and Allergology at the University Hospital of Würzburg (UKW) has now found a promising approach to combat this resistant germ. This has been published as a clinical tip in the Journal of the American Academy of Dermatology. The researchers treated two elderly patients with long-standing, infected wounds with a powder containing Lactobacillus in addition to standard care.
The probiotic preparation contains "good" lactic acid bacteria, such as those found in the body. The odour and coating of the wounds improved significantly after just a few days and new, healthy tissue appeared after one to two weeks. Pseudomonas aeruginosa was no longer detectable in the subsequent control swabs. The patients tolerated the treatment well and there were no relevant side effects. Similar improvements were also seen in other patients.
Lactic acid bacteria promote wound healing
"Lactic acid bacteria can therefore weaken harmful bacteria such as Pseudomonas aeruginosa by disrupting their biofilms, reducing inflammation and activating the cells involved in wound healing," says Dr. Tassilo Dege, lead author of the case study, interpreting the results.
Studies on models with human skin confirmed that lactobacilli weaken the biofilm of Pseudomonas bacteria and disrupt their communication. This makes the problematic bacteria less harmful. At the same time, certain signals, such as interleukin-6, stimulate important skin cells and connective tissue cells so that wound healing is supported. In animal models with mice, the researchers observed that certain metabolic products of the lactobacilli reduced the number of Pseudomonas bacteria and the inflammation in the wound.
"Our results suggest that probiotics could be a simple and well-tolerated addition to the treatment of chronic wounds without the risk of antibiotic resistance," says Professor Astrid Schmieder. At the same time, however, she warns that live probiotics theoretically harbour risks and that careful medical supervision is therefore necessary. Further studies will now investigate this simple and safe complementary therapeutic approach in more detail.
Disease patterns and treatment of the two patients
In the dermatological case observation, one patient suffered from a so-called pyoderma gangraenosum, the other from a venous leg ulcer. Both wounds were colonised with the bacterium Pseudomonas aeruginosa. After daily wound cleansing with sterile saline solution, the wound was covered with a non-adherent wound dressing (Adaptic), plus multi-layer compression in the case of the venous leg ulcer. In addition, the wound was treated daily with a preparation containing lactic acid bacteria (Vagisan with Lactobacillus gasseri and Lacticaseibacillus rhamnosus in high bacterial counts).
Publication
Tassilo Dege, Andreas Kerstan, Matthias Goebeler, Astrid Schmieder. Clinical pearl: Topical Lactobacillus application to disrupt Pseudomonas aeruginosa biofilms and promote healing in chronic wounds, Journal of the American Academy of Dermatology, 2025, ISSN 0190-9622, https://doi.org/10.1016/j.jaad.2025.12.071.